by Jocelyn M. Wood, M.A. CCC-SLP
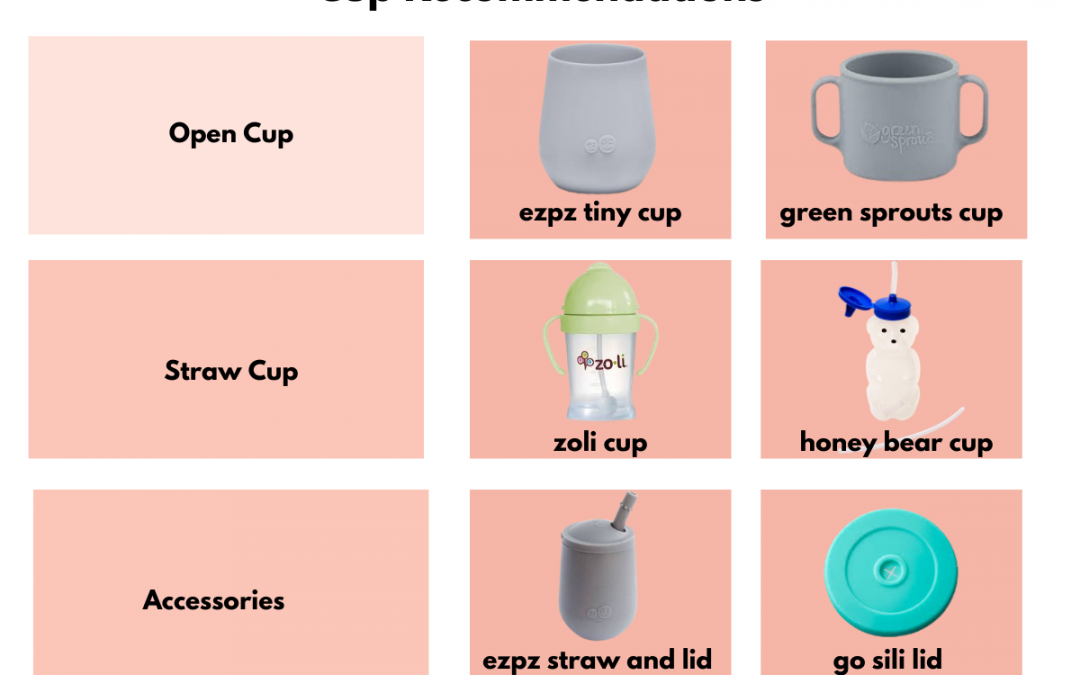
When it comes time to choose a cup for your child, parents need to consider the effect that sippy cups have on speech development. As a speech therapist specializing in oral motor development, I have very strong opinions about cup drinking. Teaching your toddler...

by Jocelyn M. Wood, M.A. CCC-SLP
These are unprecedented times we are living in. With the global pandemic ever present, many families find themselves at home, together, at all times. This presents challenges in the best-case scenario, but add in a child with a disability and you are doomed—or so you...

by Jocelyn M. Wood, M.A. CCC-SLP
You’ve heard the words early intervention before, but it seems confusing. A pediatrician tells you that they are free services for children aged birth to 3. Your friend from Gymboree tells you that the only way to qualify is to have your child evaluated right...

by Jocelyn M. Wood, M.A. CCC-SLP
During the first year of life, your new baby will take the journey that brings him from a crying ball of mush to his first words. It is exciting, breathtaking…and nerve-racking as you ponder whether all this is normal. As part of my new parenting series, I...

by Jocelyn M. Wood, M.A. CCC-SLP
The longer I work as a speech-language pathologist, the more I appreciate working with occupational therapists. I checked in with my friend Jill Loftus at Honest OT in Denver, Colorado, to find out How Sensory Processing Impacts Speech Development. It’s important to...